Each year Medicare offers its beneficiaries a chance to make changes to their Medicare coverage. This year, the dates for Medicare’s Open Enrollment are October 15-December 7, 2019.
During Open Enrollment you can change your Original Medicare A & B to a Medicare Advantage Plan, change from one Medicare Advantage Plan to another, add or change your prescription plan, or change your Medicare Advantage Plan back to Original Medicare. The changes you make will go into effect on January 1, 2020.
Medicare is not a set it and forget it plan.
Most folks do nothing, allowing their coverage to stay the same. This decision could cost them tremendously in both financial and care options.
Each drug plan and Medicare Advantage Plan can change each year. These changes impact providers and patients alike.
Premiums, copays, or other out of pocket costs may go up unexpectedly, coverage may not be as robust as in years past, healthcare provider networks may change, and terms for providers may change, limiting providers willing to work with certain insurance carriers at all. Please remember that our Mindful Transitions team does not accept ANY of the Medicare Advantage plans-only Traditional Medicare.
It is important for you to review your coverage, your needs, and your options every year.
Here are a few tips from The Medicare Rights Center to get you started:
- If you are looking for a new Part D plan, you can use the Plan Finder tool from www.Medicare.gov to compare options in your area. Before you use Plan Finder, make a list of the medications you take, the amount that you currently pay for them, and which pharmacies you like to visit. You will be able to get a sense of which plans cover the medications you need with the lowest costs and fewest coverage restrictions.
- If you are shopping for a new Medicare Advantage Plan, you can use the Plan Finder tool to compare options in your area. You can also call 1-800-MEDICARE and ask about plans in your area. Once you have a list of your available options, you can visit their websites to learn more.
- After you have researched plans and found one that you are interested in, call that plan directly to confirm what you learned online. Ask about your doctors and hospitals to check that they are included in your plan’s network. Check also that the plan includes all the drugs you need on its formulary, and that your pharmacies are in the plan’s network. Write down everything about this conversation, including the date of the conversation, who you speak to, and the outcome of the call.
- Call 1-800-MEDICARE if you decide to enroll in a new plan. This is the best way to protect yourself if there are any problems with enrollment. Write down everything about your call, including the date of the conversation, who you speak to, and any information the Medicare representative gives you during the call. Remember to confirm all the details about your new plan with the plan itself before calling Medicare.
- Be wary of solicitations and advertisements stuffing your mailbox (both snail mail and email). Medicare Advantage Plans have started sending out information about their plans, but they must follow certain rules.
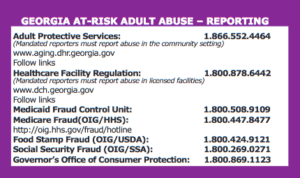
If you need additional help, please reach out to GA Cares at 1-866-552-4464 (option 4).
For more information please visit Medicare Rights Center.
All of the Clinical Social Workers are Medicare providers and accept assignment. We do not, however, accept any of the Medicare Advantage Plans. If you want to learn more about our services, please visit our FAQ page, call us at (678) 637-7166, or email us at inquiry@mindfultransitions.com